

Affiliations
ABSTRACT
Hordeolum is an acute, painful, and common eyelid disease with high prevalence. Studies have illustrated that intense pulsed light (IPL) is an effective and feasible option for meibomian gland dysfunction (MGD)-related dry eye disease (DED) and other eyelid diseases. This is the first study to evaluate the therapeutic efficacy and safety of IPL for treating patients with hordeolum. Herein, a retrospective case series is reported with three patients with hordeolum, who had successfully received IPL treatment once. The symptoms and signs of eye discomfort were significantly reduced in all three patients after IPL treatment. Moreover, no adverse events were reported. Even for child or adult patients after chemotherapy, IPL can greatly relieve the swelling and pain, and reduce the mass in size. IPL appears to be a safe, reasonable, and effective option for patients with hordeolum.
Key Words: Hordeolum, Intense pulsed light, Eyelid disease, Meibomian gland, Dry eye.
INTRODUCTION
Hordeolum is an acute and common inflammation of the eyelid margin that presents as a painful, red, and swollen round furuncle. In some cases, the episode of hordeolum is self-limited and resolves with the inflamed lesion draining spontaneously. When the infection is severe, conservative interventions including warm compresses, topical antibiotics or even incision and drainage may be indicated.1 Intense pulsed light (IPL) therapy is a non-coherent, high-intensity light source with wavelengths of 500 to 1200 nm. Recently, ophthalmologists have paid more attention to the use of IPL in treating several eye diseases. Till now, a few studies reported that IPL is an effective therapy in treating paediatric blepharitis,2 recurrent chalaziosis,3,4 ocular Demodicosis, and allergic keratoconjunctivitis (AKC).5 Similarly, hordeolum is also an inflammation of the margin of the eyelid. Here, we report three cases of hordeolum patients treated with IPL. To the best of our knowledge, this is the first study to report the therapeutic efficacy of IPL in the treatment of hordeolum, which seems to be a feasible, safe, and alternative option for hordeolum patients.
CASE 1:
A 36-year-old woman came to the clinic due to a mass of the left lower eyelid for 3 days. The mass developed during chemo-therapy after breast-conserving therapy.
The patient experienced pain and swelling. On examination, the lower eyelid was red and swollen, with a tender lump (8×6 mm) in the left eyelid region, mild conjunctival hyperaemia, and oedema. The patient was clinically diagnosed with hordeolum and received treatment of IPL. Before IPL treatment, the skin of the eyelids was anaesthetised with clear lidocaine hydrochloride ophthalmic gel, 3.5%. Ocular anaesthetic proparacaine was placed in the eye, and a protective metal eye shield was placed on the patient’s cornea and sclera. The ultrasonic gel was applied to the eyelid skin of the patient. The 3 mm circular adaptor was positioned on top of the rectangular sapphire crystal. The intensity of the IPL machine ranged from 9.8 - 13 J/cm2 according to the Fitzpatrick Skin Type Grading. The IPL treatment was directly applied to both upper and lower eyelids with 20% overlap and the patient received 10 pulses for two passes per session.3 After the treatment, the symptoms of ocular discomfort were immediately relieved, and the mass was smaller than before. On the 2nd post-therapeutic day, the pain and swelling disappeared, while the mass significantly reduced in size.
CASE 2:
A 5-year girl was referred to the clinic with an acute, red, painful, raised mass on the left lower eyelid for 3 days. She had used Tobrex (0.3% Tobramycin Eye Drops) (s.a. Alcon-Couvreur n.v., Puurs, Belgium) 4 times daily for 2 days but there was no improvement. The mass was approximately 10×5 mm, along with two pus points on the edge of the eyelid (Figure 1A). Hordeolum was definitively diagnosed and IPL therapy was performed once. Two days after the therapy, the above symptoms were significantly improved and the size of the hordeolum decreased (Figure 1B).
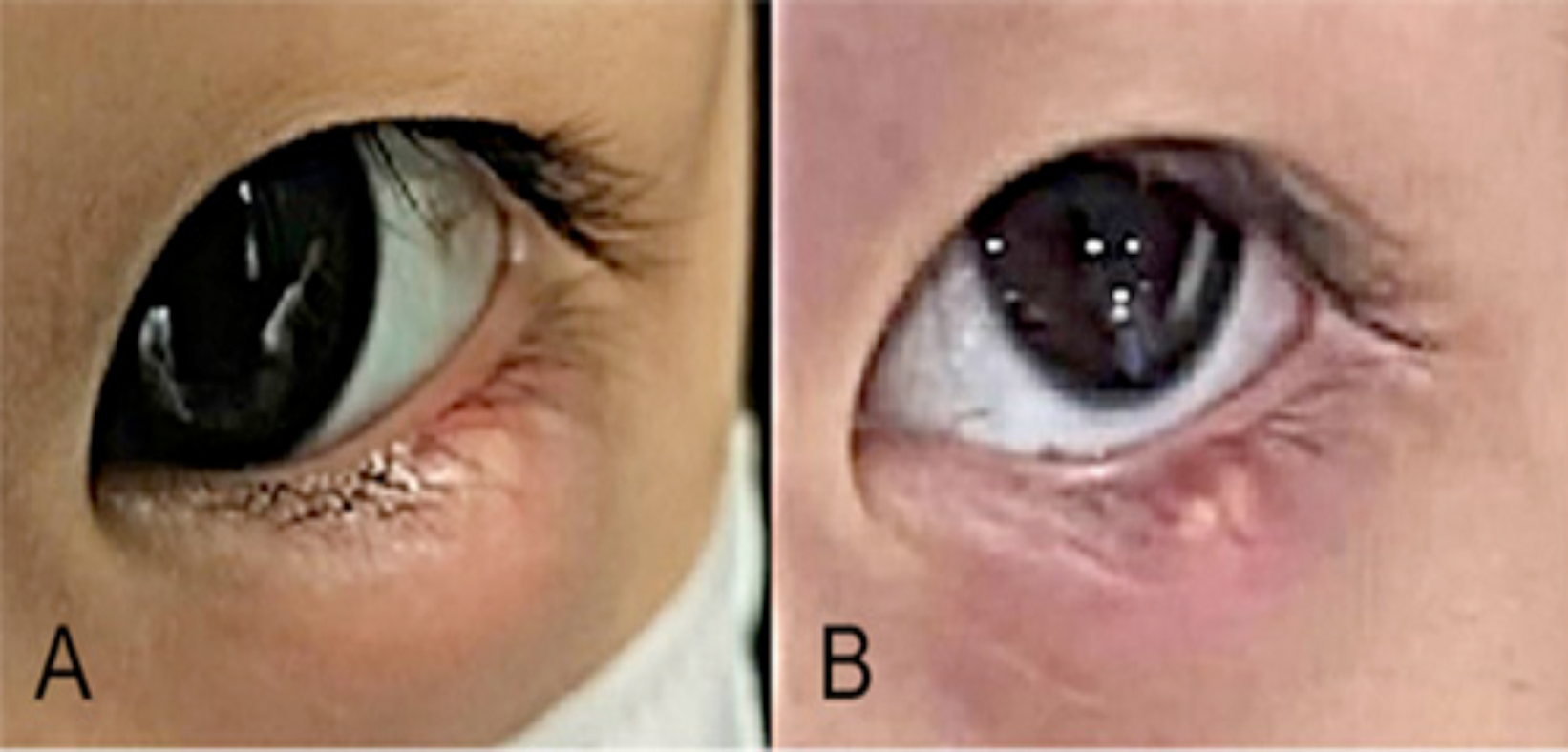 Figure 1: The clinical features of a child with hordeolum before and after the IPL treatment. (A) A 5-year girl presented with an acute, painful and red mass (10 × 5 mm) on the left lower eyelid. (B) Two days after the IPL therapy, the redness, pain, and swelling of the eyelid notably relieved, and the size of the hordeolum decreased.
Figure 1: The clinical features of a child with hordeolum before and after the IPL treatment. (A) A 5-year girl presented with an acute, painful and red mass (10 × 5 mm) on the left lower eyelid. (B) Two days after the IPL therapy, the redness, pain, and swelling of the eyelid notably relieved, and the size of the hordeolum decreased.
CASE 3:
A 35-year woman came to the clinic complaining of a red mass on the right upper eyelid with symptoms of pain, swelling, and a mild foreign body sensation. The hordeolum was about 8×5 mm and a diagnosis of hordeolum was indicated. The patient underwent IPL therapy once. One day after the therapy, the redness and pain of the eyelid disappeared and the hordeolum reduced. Two days post-therapy, the hordeolum was further reduced to 3×2 mm.
DISCUSSION
Hordeolum is a painful, red, and localised inflammation, mostly caused by obstructed orifices of eyelid sebaceous glands and S. aureus infection. The conventional measures for treating hordeolum have some limitations, including antibiotic resistance and side-effects caused by long-term use of topical steroids, such as enhanced risk of cataracts and a rise in intraocular pressure.1 Surgical incision and drainage may cause skin scarring, madarosis, and eyelid margin deformation,3 and is difficult for patients especially children who have substantial psychological distress of surgery.6 For instance, the 5-year child in Case 2, would have required surgery under the general anaesthesia, and the risks of surgery will be a concern for their parents. Moreover, it is also worth noting that the costs of surgery are usually high, which increases the economic burden. For Case 1, chemotherapy could weaken the immune system, and the healing of surgical wounds is also susceptible to be affected by chemotherapy agents.7 She received IPL treatment, and her ocular discomforts were relieved immediately. Compared with the conservative interventions, IPL was more comfortable, safe, and cost-effective as a non-surgical treatment of hordeolum, and it would be more favourable to be accepted by patients with some special conditions.
As a wide and favourable form of treatment in dermatology, increasing number of studies have found that IPL is a safe and effective option for meibomian gland dysfunction (MGD)-related dry eye disease (DED), which is characterised by latent impairment to the ocular surface8 and other eyelid diseases, including recurrent chalaziosis4 and AKC.5 Arita et al. illustrated that IPL-MGX offered an effective and low-risk treatment in reducing the recurrence rate of chalazion by enhancing MG function.4 AKC is a common disease that causes burning sensation, itching, dry eyes, and may cause limited daily activity and alter patients’ life quality.9 A retrospective study reported that IPL might be an effective treatment for AKC. AKC-related signs and symptoms improved after IPL therapy in 35 patients.5 This is the first report to investigate the successful management of hordeolum with IPL therapy, which provides a good choice for patients with hordeolum in the future clinical practice.
The mechanisms of IPL treatment were proposed to be as follows: First, the thermal effect of IPL could not only coagulate the abnormal blood vessels to reduce inflammatory cytokines but also melt clogged MG which is a vital contributor to treat hordeolum. Second, IPL plays an important role in reducing dilated vessels, and the closure of these abnormal vessels may restore the hypoxic environment that MG need. In addition, IPL may improve MG microstructure by its photomodulation effect, and decrease the inflammation of MG.10 One limitation of the study was with the lack of follow-up visits, which may have an impact on the observation of long-term efficacy. In addition, further randomised, controlled studies are required to investigate the mechanisms in IPL therapy treating hordeolum.
In summary, it is the first study to investigate the successful treatment of hordeolum with IPL. IPL treatment could significantly improve the ocular symptoms and signs of hordeolum without notable side-effects. This study offered a favourable, safe, and prospective option with high efficacy on hordeolum.
FUNDING:
This work was supported by The National Natural Science Foundation of China under Grant No. 82171023, Science and Technology Department of Jilin Province Fund under Grant No. 20210101279JC, and Bethune Centre for Medical Engineering and Instrumentation under Grant No. BQEGCZX20210XX.
PATIENTS’ CONSENT:
Patients’ consent was obtained from all patients.
COMPETING INTEREST:
The authors declared no competing interest.
AUTHORS’ CONTRIBUTION:
YR: Summarised the relevant literature and prepared the manuscript.
TH: Drafted and revised the manuscript.
DZ: Edited and corrected the academic-writing.
CL: Contributed to the conception of the study.
All authors approved the final version of the manuscript to be published.
REFERENCES